The stem cell therapy of Alzheimer's disease is to administer autologous adipose tissue-derived mesenchymal stem cells intravenously.
Dr. Ra’s research team tested animals that have Alzheimer's disease and proved the effectiveness of the stem cell treatment of Alzheimer’s disease as well as the prevention of Alzheimer’s disease.
Nature CellNature Cell (KOSDAQ: 007390) is a high-tech bio enterprise, a leader of stem cell business, stem cell drugs and treatment technology development, and stem cell culture medium cosmetics.
Furthermore, Nature Cell is a member of the stem cell network Biostar, along with Rbio, GDFI Braincell Laboratory, Stem Cell Research Institute, Stemcell Life Foundation, Bethesda Hospital, R-Japan and Medicorp, which are entities committed to stem cell research for treating incurable diseases.
Biostar Stem Cell Research InstituteBiostar Stem Cell Research Institute is jointly run by Nature Cell and RBio, the adult-derived stem cells research firm.
Posts published in “Research”
Antiherpetic Medications May Reduce Risk for DementiaShare this content:linkedingoogleEmailPrintAntiherpetic medications, either overall or individual antivirals, were associated with decreased risk of developing dementia.
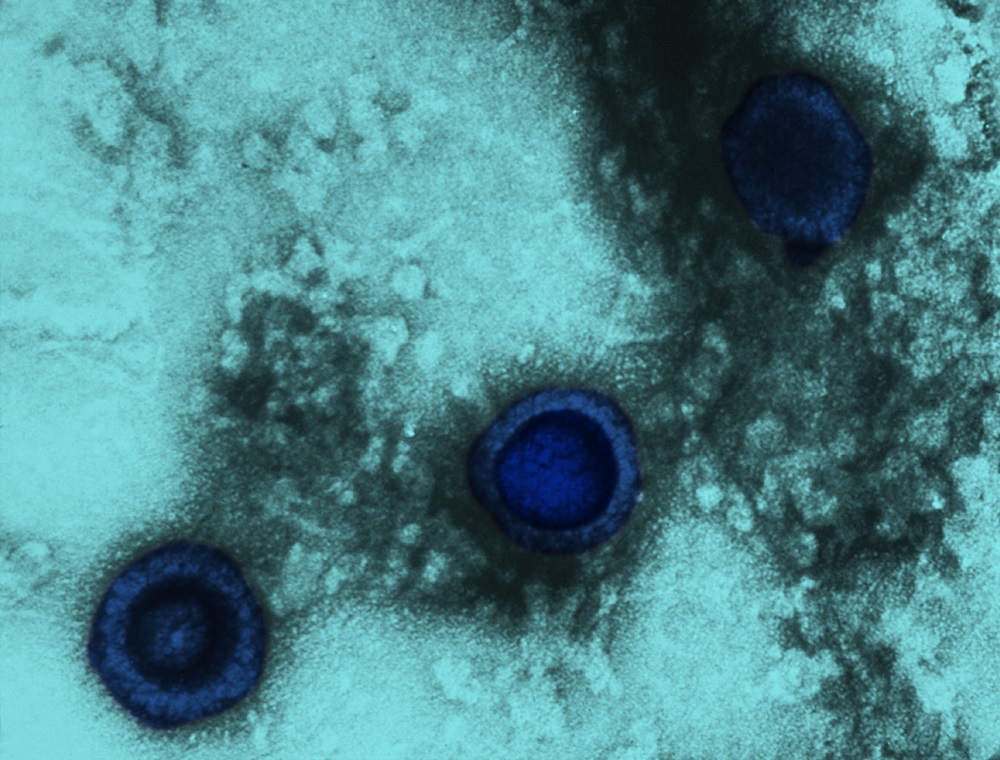
Individuals with herpes simplex virus (HSV) infections may have a 2.56-fold increased risk for dementia and the use of antiherpetic medications was associated with a decrease in dementia risk, according to research published in Neurotherapeutics.1A retrospective cohort study using Taiwan's National Health Insurance Research Database identified 8362 patients with new HSV infections and 25,086 randomly selected sex- and age-matched controls without HSV.
The use of claims data allowed patients with dementia to be identified but no data on severity or stage were available, nor were data on antiherpetic treatment durations.
There were no imaging or other laboratory data available, so investigators relied on physician diagnosis.
Furthermore, the investigators noted that while “several community studies have revealed that Alzheimer dementia is the most common cause of dementia, followed by vascular dementia, and mixed or other dementias,”2-4 most of the dementias in this study were other types of dementia.

Genetic mutations in two previously unrecognized genes, the microtubule-associated protein tau (MAPT) and BNIP1 genes, are associated with elevated risk for amyotrophic lateral sclerosis (ALS).
As seen in other neurodegenerative diseases, abnormal accumulation of toxic proteins seems to play a role in ALS onset and progression.
Different mutations in tau protein previously were associated with other neurodegenerative diseases, such as Alzheimer’s.
However, the specific mutation identified in this study was associated only with ALS, and not with the other diseases included in the study.
Genetic mutations that modestly elevate risk for ALS were identified with more than two dozen different genes.
In other words, is dominantly inherited AD the same or different from sporadic AD?
The findings to date indicate that despite having different causes, familial and sporadic AD on the whole share the same pathophysiology and progression.
Autosomal-dominant and sporadic AD have different triggers, but converge on the same pathophysiologic process.
People with a familial AD mutation (red lines) experience more aggressive amyloidosis than do people with sporadic AD (blue lines).
ADNI participants had more years of education than DIAN participants on average, and they were all from North America whereas DIAN is worldwide.

A recent study investigated whether adults with congenital heart disease have an increased risk of developing dementia.
Congenital heart disease is a heart abnormality or defect present at birth.
Occurring in approximately six to ten per 1000 births, congenital heart disease is the most common malformation in newborns.
Therefore, attention is now being paid to common morbidities (co-occurring disease) acquired by adults with congenital heart disease.
A known adverse outcome associated in children born with congenital heart disease is neurodevelopment deficits during childhood and early adulthood.

It is well known that memory problems are the hallmarks of Alzheimer's disease.
"The mice develop Alzheimer's disease in a very close manner to the human patients with early-onset form of the disease.
The results indicate that caffeine alters the behaviour of healthy mice and worsens the neuropsychiatric symptoms of mice with Alzheimer's disease.
In mice with Alzheimer's disease, the increase in neophobia and anxiety-related behaviours exacerbates their BPSD-like profile.
"Our observations of adverse caffeine effects in an Alzheimer´s disease model together with previous clinical observations suggest that an exacerbation of BPSD-like symptoms may partly interfere with the beneficial cognitive effects of caffeine.

In Alzheimer’s, scientists have hypothesized that dying brain cells break apart and release proteins, including tau, which then form the tangles that are a hallmark of the disease.
New research from Washington University in St. Louis shows, however, that tau secretion is actually an active process, not a byproduct of cell death—findings that could refine tau-targeting treatments for Alzheimer’s.
A variety of approaches are in the works to address the dearth of new Alzheimer’s treatments.
Other methods include targeting genetic variants in neurological cells to boost the immune system’s ability to fight Alzheimer’s.
"Our results showing that tau production is increased suggest that we might want to target tau production therapeutically."

Alzheimer's disease: patients exhibit changes in certain blood lipids that are typical of premature ageing.
Credit: Medical University of Vienna The neurodegenerative condition Alzheimer's disease is the most common cause of dementia.
They were able to show that normal, age-related changes in blood levels also occurred in the Alzheimer's patients but to a significantly greater extent.
Explore further: New forecast shows 6 million with Alzheimer's disease, cognitive impairmentMore information: Fabian Dorninger et al.
Alterations in the Plasma Levels of Specific Choline Phospholipids in Alzheimer's Disease Mimic Accelerated Aging, Journal of Alzheimer's Disease (2018).

ARTICLE IN BRIEFNeurologists who specialize in end-of-life and palliative care discuss a proposal to develop an advance care directive for people with dementia.
[See “Advance Directive for Dementia” for a sample of that approach.]
HOW TO INCORPORATE INTO CAREIn interviews with Neurology Today, several independent experts in neurology and palliative care agreed with this approach, and to varying degrees, they said, they incorporate these principles into discussions with their patients.
Dr. Kluger emphasized that early and ongoing goals-of-care conversations are probably more important than “the specific piece of paper” with an advance directive for dementia.
“Every person with dementia has a different course,” he said, elaborating on its unpredictability and the difficulties of capturing all relevant scenarios in a dementia-specific advance directive.

Immune cells in the brain have a trigger, and when it is pulled, it prompts immune cells to degrade toxic β-amyloid (Aβ) proteins.
This new finding, from Sanford Burnham Prebys Medical Research Institute (SBP), helps explain why a faulty trigger appears to raise the risk of Alzheimer’s disease.
Increasing the genetic expression of the trigger—a way of pulling the trigger more often—could prevent or reduce the severity of Alzheimer’s disease and other neurodegenerative disorders.
The second study (“Elevated TREM2 Gene Dosage Increase Reprograms Microglia Responsivity and Ameliorates Pathological Phenotypes in Alzheimer's Disease Models”) added TREM2 to a mouse model with aggressive Alzheimer's disease.
"We could use brain immune cells to solve what's becoming a public health crisis."
